Improving Outcomes for the Non-Compliant Patient/Resident/Person
When you find yourself in a conflict with the patient, one of the best techniques you can use is to separate the person from the problem. How do we do this? In these situations, it becomes a conflict between “my way” and “your way”. And we just keep battling until either one of us wins or we both get more frustrated. This doesn’t do the patient any good and it wastes our time. Let me give you an example. The patient comes in and hasn’t been taking their medication. Usually we would say, “Why haven’t you been taking your medication?” And what we really mean is, “Why are you being a problem?” This approach rarely works.
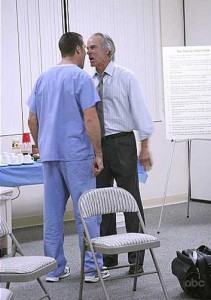
So, instead you might want to say to the patient, “How are you and I going to solve the problem of the medicine getting into you?” The problem becomes the third person in the room. You have separated the person from the problem. Now the person isn’t the problem, the problem is the problem. This takes the pressure off the situation and the two of you can begin to brainstorm to figure out a workable solution.
One quick note before you start brainstorming, make sure you understand what is the real issue. Are they not taking their medicine is because they can’t afford them? Are they not taking their medicine because they don’t like the way it makes them feel? Or are they not able to cut the pill in half or open the medicine bottle? These are just a few examples of the many reasons people might not be taking their medications. Figure out what the real issue is and you’ll be able to solve the problem together.
Have a kind and respectful day.



Mark Cruz on Wed, 2nd Dec 2015 3:33 pm
Hello Ms Kind. I am a student at Grand Canyon University. My professor is a colleague of yours, Karen Rice. She suggested that we explore your website. Several sections were very intriguing. In particular, the section about dealing with angry patients was good to read. Your suggestion to remove the patient from the problem in order to diffuse the situation is a great idea. I have found that there seems to be an increased number of events in my hospital regarding expressions of anger from patients and family members. Are you finding this to be the same throughout the country? Do find that it is due to failed expectations, poor communication, staff fatigue or is it something altogether different? Also wanted to add that I find that most nurses and doctors fail to ask for help because they often are too focused on a task or disease process to recognize that the patient is showing signs of anger. Do you encounter this often when dealing with clinicians?
Viki Kind on Mon, 7th Dec 2015 8:32 am
Nice to meet you. Please tell Karen thanks from me. Yes, I think it is all of these and more: failed expectations, poor communication and staff fatigue. I think there is a systems problem where one piece of the system breaks down which influences the next part of the system until the entire circle of communication between participants is affected. What I am hearing the most right now is staff fatigue, anger, and increased de-personalization. Medical professionals are so emotionally exhausted, they can’t connect to the patients/families. And this upsets the patients/families who then get angry which then makes it more difficult for the staff. You can see the viscous circle. Here is a link to an article on physician fatigue: http://www.medscape.com/viewarticle/855233?src=wnl_edit_medn_wir&uac=7563PN&spon=34&impID=910736&faf=1 I was shocked to see that in just 3 years, physicians reporting being seriously emotionally exhausted went from 36%-46%. A huge increase.
I have a great deal of empathy for the doctors, nurses and other professionals. The healthcare system requires them to work faster and faster, and then penalizes them when they can’t be perfect robots working on overdrive. There is no way to go faster and not effect the communication experience between the professional and patient. As an ethicist, I don’t understand how doing healthcare faster became a more valuable outcome than doing healthcare well. I can’t imagine anyone explicitly saying to their brain surgeon, “Go as fast as possible when you are operating on me today.” It is ridiculous and it is damaging our dedicated professionals.
You also might want to look at the work Dr. Pamela Wible is doing to help suicidal doctors. http://www.idealmedicalcare.org/blog/ She has a new TED MED talk coming out in January.
The other basic issue is that professionals aren’t taught good communication strategies for dealing with angry patients. I am doing a lot of talks lately on conflict management for the professional. When the professionals don’t have conflict management communication tools, of course it increases their stress level and decreases their willingness to engage with the angry patient. The other part of the communication cycle is that professionals don’t set realistic expectations. I see a lot of false hope being offered because it is easier to give false hope then to say the bad news. So then, when the patient doesn’t get “better,” the patient/family gets angry. I work as a bioethicist but before that I have had extensive training and experience in mediation. Those tools have served me as much as my bioethics education/experience.