Interview with Ron Bruno, Executive Director of Morningside Retirement and Health Services, on Feb. 24th, 9AM pst.
February 18, 2010 by Viki Kind
Filed under Kind Ethics Radio
On February 24th, 9AM pst, I will be interviewing the executive director of Morningside Retirement and Health Services, Inc. (MRHS) which serves elderly residents of Morningside Gardens, a 982 unit, multi-racial, middle income housing development in West Harlem. It consists of six high-rise buildings and approximately 1,700 residents. More than 50% of the households include a resident over the age of 60. Many of the older residents have lived in the Gardens since it opened for occupancy in 1957 and have “aged in place.” As a result, the complex has become what is known as a “NORC”–a Naturally Occurring Retirement Community–with a large population of elderly people with special needs. The mission of MRHS is twofold. We aim to: * HELP frail and at-risk elderly residents of Morningside Gardens remain in their own homes comfortably, safely, and with as much independence as possible for as long as they can. * PROVIDE programs which promote health and provide opportunities for education, socialization and recreation for all older residents of Morningside Gardens, with particular attention to the special needs of the infirm, homebound, and isolated.
The mission of MRHS is twofold. They aim to:
• HELP frail and at-risk elderly residents of Morningside Gardens remain in their own homes comfortably, safely, and with as much independence as possible for as long as they can.
• PROVIDE programs which promote health and provide opportunities for education, socialization and recreation for all older residents of Morningside Gardens, with particular attention to the special needs of the infirm, homebound, and isolated.
Services
MRHS now serves about 300 residents a year with an on-site staff consisting of three social workers, a full-time geriatric nurse, two part-time home health aides, a consulting psychiatrist, and approximately 150 volunteers, most of whom are elderly themselves. The professional staff provides an array of health care and social work services, which include case management, nursing care, psychiatric consultations, doctors ‘house calls’ for the homebound, entitlements counseling, home evaluations, home care and hospital discharge planning, liaison with families, lawyers, physicians, and financial planners.
MRHS’ Doctors Home Visiting Program is staffed by geriatric fellows who provide medical care to the homebound elderly under the supervision of the Division of Geriatric Medicine of St. Luke’s/Roosevelt Hospital Center. In collaboration with the health care team, MRHS’ consulting psychiatrist provides psychiatric evaluations, therapeutic counseling, and medication monitoring.
In addition, educational, recreational, and social activities are offered — almost all of them planned and led by elderly volunteers. Volunteers also provide direct, concrete assistance to their neighbors, such as shopping, escorting, visiting, bill-paying, and reading correspondence.
http://mrhsny.org
Phone:
(212) 666-4000
February 14th-21st is “Alzheimer’s and Dementia Staff Education Week”
February 15, 2010 by Viki Kind
Filed under Ethics In Action
February 14th-21st is ALZHEIMERS AND DEMENTIA STAFF EDUCATION WEEK
This week is designed to bring awareness to the importance of both staff educators and their direct care staff being trained and certified in dementia care. For more information and free Tool Kit (download), visit www.nccdp.org, National Council of Certified Dementia Practitioners.
I want to thank all those who take such good care of our loved ones and who strive to be educated and updated about the new research and best practices in dementia and Alzheimer’s care.
Take time this week to acknowledge those experts who are making a difference in your loved one’s lives.
Have a kind and respectful day.
Life’s Simple 7 from the American Heart Association – February is American Heart Month
February 11, 2010 by Viki Kind
Filed under Ethics In Action
February is American Heart Month.
The American Heart Association has a new feature and tool on their website called: Life’s Simple 7.
1. Get active
2. Eat better
3. Lose Weight
4. Stop smoking
5. Control cholesterol
6. Manage blood pressure
7. Reduce blood sugar
I would encourage you to take the 7 minute assessment to take control of your heart health.
http://mylifecheck.heart.org/PledgePage.aspx?NavID=5&CultureCode=en-US
Then take the pledge to embrace Life’s Simple 7 at “My Life Check” at
http://mylifecheck.heart.org/Default.aspx?NavID=1&CultureCode=en-US
Have a kind and respectful day.
Moira Fordyce’s recommends the resources on the American Geriatric’s Society website
February 8, 2010 by Viki Kind
Filed under For Patients & Families

I was speaking with Moira Fordyce from the California Coalition for Caregivers and she told me about the wonderful resources available at the American Geriatrics Society website. http://www.healthinaging.org/public_education/index.php The great thing about this website is that you know you can trust this information because it is coming from physicians who specialize in helping the aging patient and their loved ones.
You may also want to take a look at the California Coalition for Caregivers as they are an advocacy organization and are fighting to make sure that resources and protections are in place for our aging population. http://www.californiacrc.org If you live in California, they will send you alerts when it is time to contact your local representatives about an upcoming bill or iss
Lastly, you might want to download some of the legal handbooks for senior care from Bet Tzedek Legal Services at http://www.bettzedek.org/publications.html#guides.
Below I have listed the topics from the American Geriatrics Society’s site. They have Tip Sheets, What to Ask Your Doctor, and General Aging Topics. It is like having a trusted friend to turn to for help. Have a kind and respectful day and enjoy the resources.
Latest Foundation Tip Sheets
Caregivers
Guide to Advance Directives
Tips For Avoiding Caregiver Burnout
Healthy Aging
Advice for Improving Your Memory
Cognitive Vitality
“Geriatric Syndromes”
Good Health in Later Life for Older Men
Good Health in Later Life for Older Women
Improving Communication with Your Healthcare Provider
Overcoming Challenges to Healthy Aging
Persistent Pain Tips
Holidays
Tips for Beating the Holiday Blues New!
Top 10 Healthy New Year’s Resolutions for Older Adults New!
Safety
2009 H1N1 Flu (“Swine Flu”) Tips
Emergency Preparedness Tips
Falls Prevention Tips
Home Safety Tips
Hot Weather Safety Tips
Safe Travel Tips
Safe Sex Tips
Safety Tips for Seniors Considering Visits to Retail Medical Clinics
Walking Tips
Winter Safety Tips
Spanish
Spanish Language Health Tip Sheet: “Manejo del “Dolor Persistente” en la Tercera Edad”/“Managing Persistent Pain In The Elderly”
Surgery
Hip and Knee Joint Replacement Tips
Vaccinations and Medications
Avoiding Overmedication and Harmful Drug Reactions
Vaccination Tips
What to Ask?
Questions for Your Healthcare Provider
How We Age
• Physical Activity
• Prevention
Health Care Decisions and Issues
• Health Assessment
• Health Care Settings
o Community-Based Care
o Hospitalization
o Nursing Home Care
• Complementary and Alternative Medicines
• Drug Treatment
• Elder Mistreatment
• Ethical and Legal Issues
• Pain Management
• Palliative Care and Hospice
• Rehabilitation
Elder Health at Your Fingertips
• Cancer
• Diabetes
• The Digestive System
o Disorders of the Digestive System
o Disorders of the Mouth
• The Heart, Lungs, and Blood and Circulation
o Anemia and Other Blood Disorders
o Breathing Problems
o Fainting (Syncope)
o Disorders of the Heart and Circulatory System
o High Blood Pressure
• Hormone Disorders
• Joints, Muscles, and Bones
o Back Pain
o Falls
o Foot Problems
o Osteoporosis
o Walking Problems
• Mental, Neurological, and Psychological Conditions
o Anxiety
o Delirium (Sudden Confusion)
o Dementia
o Depression
o Diseases of the Nervous System
o Dizziness
o Mental Retardation
o Personality Disorders
o Psychological and Social Issues
o Psychoses (Delusions and Hallucinations)
o Sleep Problems
o Substance Abuse
• Nutrition
• Sexuality and Sexual Concerns
o Gynecological (Female) Disorders
o Prostate Disease
o Sexual Problems
• The Senses
o Hearing Loss
o Vision Loss and Other Eye Diseases
• The Skin
o Pressure Ulcers (Bed Sores)
o Skin Diseases
• The Urinary System
o Kidney Problems
o Urinary Incontinence
Topics at a Glance
How We Age
• The Aging Process
• Trends in the Elderly Population
• Physical Activity
• Prevention
Health Care Decisions and Issues
• Talking to Your Healthcare Providers
• Health Assessment
• Health Care Settings
o Community-Based Care
o Hospitalization
o Nursing Home Care
• Complementary and Alternative Medicines
• Drug Treatment
• Elder Mistreatment
• Ethical and Legal Issues
• Insurance, Financing, and Costs of Health Care
• Pain Management
• Palliative Care and Hospice
• Rehabilitation
Elder Health at Your Fingertips
• Cancer
• Diabetes
• The Digestive System
o Disorders of the Digestive System
o Disorders of the Mouth
• The Heart, Lungs, and Blood and Circulation
o Anemia and Other Blood Disorders
o Breathing Problems
o Fainting (Syncope)
o Disorders of the Heart and Circulatory System
o High Blood Pressure
• Hormone Disorders
• Infectious Diseases
• Joints, Muscles, and Bones
o Back Pain
o Falls
o Foot Problems
o Osteoporosis
o Problems with Joints, Muscles and Bones
o Walking Problems
• Mental, Neurological, and Psychological Conditions
o Anxiety
o Delirium (Sudden Confusion)
o Dementia
o Depression
o Diseases of the Nervous System
o Dizziness
o Mental Retardation
o Personality Disorders
o Psychological and Social Issues
o Psychoses (Delusions and Hallucinations)
o Sleep Problems
o Substance Abuse
• Nutrition
• Sexuality and Sexual Concerns
o Gynecological (Female) Disorders
o Prostate Disease
o Sexual Problems
• The Senses
o Hearing Loss
o Vision Loss and Other Eye Diseases
• The Skin
o Pressure Ulcers (Bed Sores)
o Skin Diseases
• The Urinary System
o Kidney Problems
o Urinary Incontinence
Interview with Lauren Gershen, “Answering your questions about Long Term Care Insurance”, Feb. 5th, 9AM pacific
January 21, 2010 by Viki Kind
Filed under Kind Ethics Radio
Call in to listen live at (347) 945-5152 or listen online at blogtalkradio.com/kindethics.
Lauren specializes in offering multiple solutions to Long Term Care Planning. She is certified and licensed in 10 different states, and introduces her clients only to those companies that are top rated, financially solid, and experienced in writing and underwriting long term care insurance. “It is important to maintain your quality of life and to have peace of mind knowing that you have a plan that will help you maintain your control and independence when you need it to in an affordable manner, and postpone or even avoid the need for institutionalization.”
Lauren resides in La Quinta, California and is a graduate of UCLA. She has first hand experience of the potentially significant impact that not having a plan can have on you, your family and loved ones, and your retirement portfolio. Her practice focuses specifically on the issue of long term care insurance, plan design & implementation, comparison and analysis, and finding the insurance product and company that is right for you. Her primary mission is to educate people on the value of having protection against the high costs of long term care while choices are still available. After working with Lauren, clients appreciate the value of being able to make “well-informed” YES or NO decisions about how to approach this critical life planning issue. In a caring and supportive way, she can assist you in customizing an appropriate and affordable plan to meet your individual or group needs.
Lauren works very closely with other professionals including elder law attorneys, financial planners and CPA’s to establish a plan that takes into consideration your circumstances and ability to pay. She also assists her clients with life insurance planning, and guides them in sifting through the maze of selecting the appropriate medicare supplement insurance plan.
Lauren actively supports the Alzheimers Association and volunteers her time to provide seminars and workshops to professionals and civic organizations. An astonishing statistic…..”One in six Baby Boomers who reach age 55 will develop some kind of dementia, including Alzheimer’s.”
Lauren actively represents the following top rated LTC insurance companies:
Authorized to offer AARP endorsed Long Term Care Insurance, Prudential, Genworth Life, MetLife, John Hancock, Mutual of Omaha and Allianz.
Lauren V. Gershen CLTC
Planning For Quality of Life
Long Term Care Planning & Insurance Specialist
LGershen@aol.com
(760) 777-9061 Office
(760) 777-9062 Fax
Have a kind and respectful day.
Improving the Medical Experience of the Person struggling with Alzheimer’s or other memory loss
January 17, 2010 by Viki Kind
Filed under For Healthcare Professionals
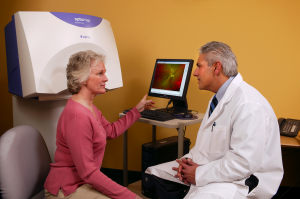
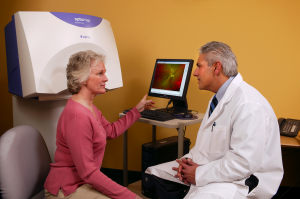
When a person with Alzheimer’s or dementia is going to have a medical test or procedure, how can we help the person to feel less frightened and to minimize any suffering? If the patient is struggling to understand what will be happening to them, do a practice run-through and show the person the room where the test will happen. Or find a book with pictures that will help him understand what you are talking about. If the person with diminished capacity is afraid of being alone, you may want to introduce him to the nurses who will be working that day. For my dad, we tape-recorded the doctor’s explanations so he could listen to the information over and over again until he felt more comfortable.
Another thing to keep in mind is that the patient may be experiencing symptoms that affect his or her participation. These symptoms could be pain, side effects of medications, loss of hearing or sight, lack of sleep, an undiagnosed illness and grief, to name a few. Find out what can be done to relieve these symptoms to make it easier for the individual to participate in the process. Ultimately, our goal is to think about the quality-of-life questions from the person’s perspective as he or she will experience the consequences of our decisions.
Have a kind and respectful day.
What Do I Do When Someone is Grieving?
A doctor stopped me in the hall the other day and asked what he could do to comfort his brother whose son had just died. He told me that the son was only 25 and had died in a car accident. The doctor said that when he talked to his brother, all his brother had done was to scream and yell at him. He didn’t understand why his brother reacted that way when all he was trying to do was to help.
As I sat down, I could see this doctor’s grief and pain. He was suffering for both the death of his nephew and because he couldn’t find a way to be supportive of his brother. He didn’t understand that grief, especially the early stages of grief can show up in many different ways. His brother wasn’t angry at him, he was angry that his son was dead. But he was taking it out on those around him. That is normal.
Everyone is different in their grief. Some people cry. Others get silent. Some can’t eat while others can’t get out of bed. Any emotion is okay when someone is in grief. And the grief will change as time goes on. When my Dad died, at first I was very quiet and wanted to be left alone. Then I couldn’t stop crying and needed people’s support. And now, years later, it is still an ache deep in my heart.
So how can we help?
1. There are no magic words to make the person feel better. Just say, “I am sorry for your loss.” Now I know you want to make them feel better, but trying to find the perfect words won’t help, but listening does. Listening is very healing.
2. So your next step is to listen, truly listen. If they start talking about their grief, don’t jump in with your own story about the loss you suffered in the past. It is not about you. It is about being present with them and their suffering. I admit that listening is hard. But try to sit still, be quiet and give them this gift.
3. The other thing you can do is to “normalize” their grief. What does this mean? The grieving person would like to be reassured that what they are feeling is normal and to feel less alone with their sorrow. So if they say, “I am so angry at _______.” You can say, “It is normal to be angry. That is a part of the grief process.” Any emotion is normal. That is grief.
4. Don’t be surprised if they don’t want to talk about their loss. Sometimes people need a break from their grief and would just like to have a normal conversation with you. In some cultures and families, grief is a private matter so please respect this and continue to be a good friend.
5. Lastly, if you are a healthcare professional, is it okay to cry with your patient? Of course it is. Sharing a few tears with someone else is a sign of compassion and understanding. But do not cry so hard that the patient then has to comfort you.
Have a kind and respectful day.
Teaching your Patients How to be Good Patients
January 7, 2010 by Viki Kind
Filed under For Healthcare Professionals
 Time is limited and the patient keeps talking and talking. What can you do? I realize that patients aren’t taught how to be good patients. So it is up to us to teach them. I have three recommendations for you.
Time is limited and the patient keeps talking and talking. What can you do? I realize that patients aren’t taught how to be good patients. So it is up to us to teach them. I have three recommendations for you.
Recommendation #1 Have them write out what they want to talk about before their appointment. Now I am sure you have heard this before, but the part that most doctors miss is to get them to prioritize their questions. I tell them to circle the most important 2 questions they want to discuss with you. Otherwise you just get a long list of random questions without any sense of what they truly want you to focus on. Patients understand that you can’t answer all of their questions but they will be satisfied if you take care of the most urgent issues. I have a questionnaire form, Viki Kind’s Office Form that you can download to help you help the patient. I encourage you to give copies to your patients to keep at home so they can fill them out before their appointment. If they haven’t filled one out before they arrive, then have them work on it while they are in your waiting room. In the medical practice I used to manage, we had a clipboard and form all ready for the patient when they checked. This is an easy way to be more efficient and to increase patient satisfaction.
Now some of you might be thinking, “Good, I don’t have to spend time listening, I can just read their list.” Well, you can if you want but your patient will be angry and non-compliant. If your patient doesn’t trust you or trust that you care about them, they won’t heal as fast or follow your instructions.
Here is Recommendation #2. It is up to you to build a caring relationship with them and you do that through compassionate dialogue, not a monologue. The act of listening has its own healing properties.
Recommendation #3 The other thing you need to educate patients about is to stop asking you the, “Oh by the way…” question as you are about to walk out the door. You need to tell them up front to ask you the most important questions at the beginning of the appointment or else you won’t have to time to address their concerns. Of course, this is a hard habit to break for patients and you will have to give them time to learn to be more direct with you.
Bonus Information: Unfortunately, some of these techniques will not work with certain cultures as they use a form of indirect communication which dances around the topic and takes longer as the only way they know how to communicate. But for most of your patients, these techniques will help you manage your time while caring for your patients.
Have a kind and respectful day.
3 Secrets to Getting the Most Out of Your Dr.’s Appointment
January 7, 2010 by Viki Kind
Filed under For Patients & Families
 Do you feel like the doctor doesn’t have enough time to listen to your complaints? Is it frustrating to leave the doctor’s office and realize you didn’t get your questions answered?
Do you feel like the doctor doesn’t have enough time to listen to your complaints? Is it frustrating to leave the doctor’s office and realize you didn’t get your questions answered?
Let me tell you what is going on and you aren’t going to like it. The doctor has about 12 minutes to listen to you, exam you, figure out what is wrong with you and put together a plan to help you get better.
I can hear you saying, “But 12 minutes isn’t enough.” Of course not, but that is the reality of medicine today.
You can complain but if you are smart, you can learn the three simple steps below to get the most out of your doctor’s appointment.
Here is Secret #1. You have to think like a doctor. Doctor’s think in an organized manner, so we have to give them our information in an organized way. Doctors usually play a guessing game with us as they try to figure out what is our “chief complaint”. But these questions are just wasting our precious minutes. The more organized and prepared you are for your appointment, the better.
Here is Secret #2. The doctor will make more time for you if he likes you better. And if your doctor likes you, you will get better care. I know it doesn’t seem fair but that is just the way it works.
Secret #3 is to make sure you are nice to all of the office staff. They can make it easier or more difficult for you to get in to see the doctor. They control his schedule. So, be kind to them and say, “Thank you.”
Now let’s make it easy for the doctor to help you.
Step 1. Write down all of your medications, occasional cold medicines, vitamins, herbal medicines, natural supplements, etc. And I mean everything. Even things you don’t think are important may be very important to your health. The doctor can’t protect you from things that he doesn’t know about, so write them down. If you don’t want to write them down, then bring all of them to the appointment with you.
Step 2. Write down how you are feeling. Why are you coming to see the doctor? Tell him what is hurting you, bothering you or any other physical complaints? Write down the new symptoms first and then write down the problems that are ongoing.
Step 3. Write down your questions and then circle the 2 most important questions. The doctor doesn’t have time to answer all of your questions so it is up to you to keep the doctor focused on what is most important to you.
And a Bonus Secret, if you want to make the doctor angry, keep your most important question a secret until the end of the appointment, and as the doctor is walking out the door say, “I have one more question …” If you wait until the end for this “Oh by the way” question, the doctor will only have one minute left to answer it. Please, write down this most important question so the doctor can spend time helping you.
If you would like, I have created a form for you to use each time you go to the doctor, Viki Kind’s Office Form for getting more from your doctor. Sign up for my newsletter and I will send you new support tools once a month. Print out a couple of copies so you have them ready before your next appointment.
Have a kind and respectful day.
Interview with Lise Marquis from “A Place for Mom” – Providing senior care and housing options
January 4, 2010 by Viki Kind
Filed under Kind Ethics Radio

Interview with Lise Marquis from A Place for Mom on January 21st, 1PM pacific, 4PM eastern on BlogTalkRadio.com/kindethics. Call in to listen live and to ask your questions at 347-945-5152. Or listen later to the show at BlogTalkRadio.com/KindEthics
The Search for Senior Care….Simplified and FREE
Your personal Eldercare Advisor is Lise Marquis
866-691-2427 (local office) 760-207-9405 (mobile) lisem@aplaceformom.com
ABOUT “A PLACE FOR MOM” (and DAD)
They provide a free comprehensive resource for senior housing and care options to families in need. Each day thousands of families are faced with the unique and complex challenge of finding appropriate elder care. The array of choices and decisions to make can be overwhelming and families are left with too many unanswered questions. A Place for Mom will provide you and your family with one-on-one guidance during this difficult process.
They provide senior care and housing options in the following areas:
Independent Retirement Living
Assisted Living
Alzheimer’s & Dementia Care
Respite Care
Skilled Nursing
Home Care
Residential Care (Board & Care) Homes
Hospice
They also provide resources for:
Financing/VA Aid & Attendance
Legal Services
In Home Therapy Services
Support Groups/Professional Organizations
Touring Checklists
Some kind words:
“Hi Lise – Just wanted to thank you for the excellent referrals for my mom.
I am so impressed with you and “A Place for My Mom”. Thanks for making a difficult task SO MUCH EASIER!”
“Dear Lise, This has been the most stressful week of my life, but I could NEVER have gotten through it without you. You are truly a god send, and I will never forget how much you helped me.”
“Lise, I will pass your name along to everyone I talk to that needs a compassionate, caring person to help them in finding a place for their very special loved one.”
A Place for Mom is the nation’s largest eldercare referral network. They help hundreds of families every day. Their consultation is provided at no cost to families, as their partner communities and homes reimburse them for our services.
Have a kind and respectful day.


